
AI Revenue Cycle Automation Platform

End-to-End AI Platform For Intelligent Revenue Cycle
CombineHealth’s proprietary agentic and generative AI technology is built on 20+ years of healthcare data and trained on billions of medical records making it the most advanced and comprehensive revenue cycle automation platform.
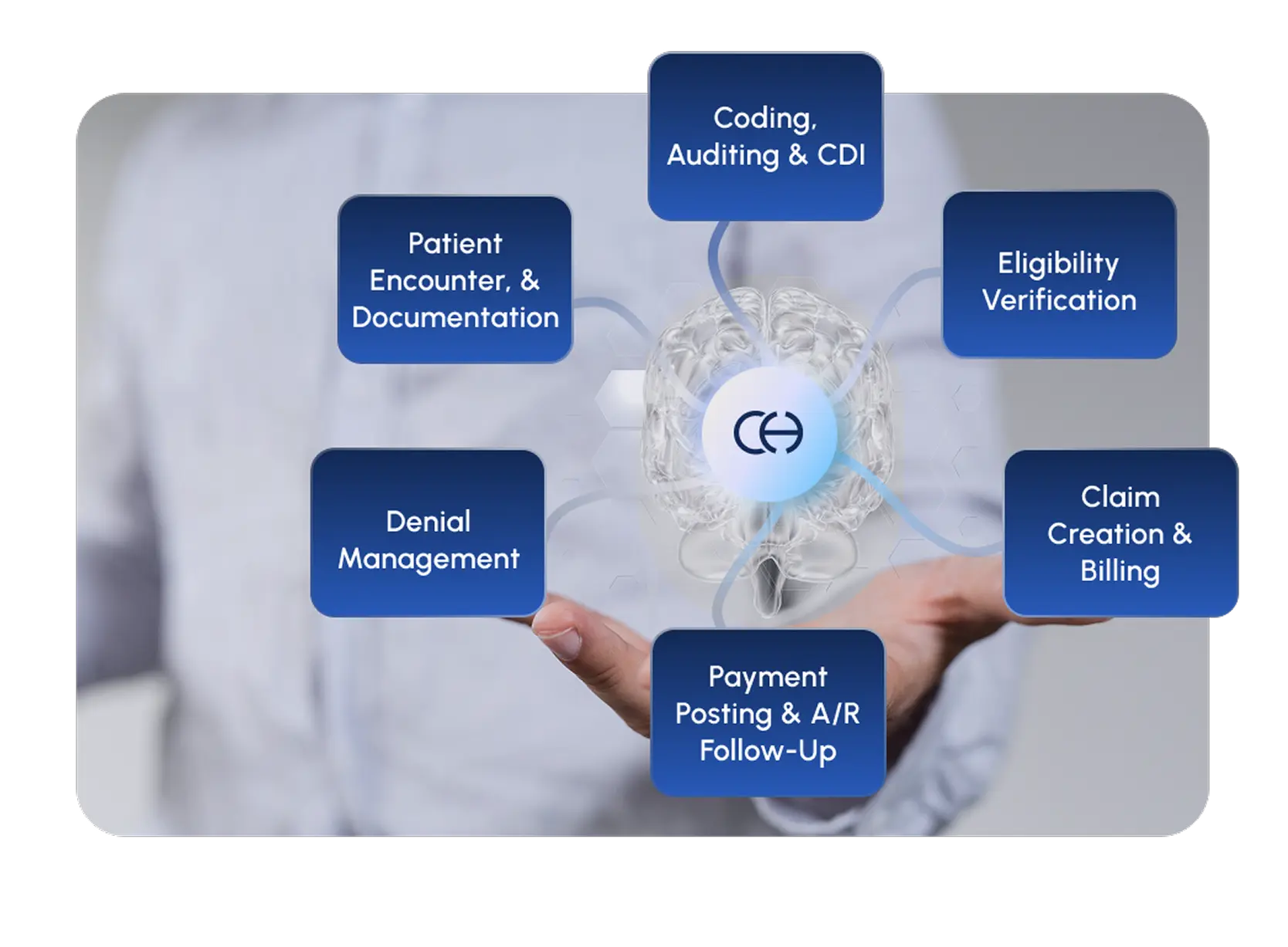
Complete Revenue Cycle Management
Our platform unifies every step of revenue cycle, from eligibility verification to collections, into a seamless process powered by AI
- Reduce denials
- Tighten your CDI process
- Increase coding accuracy
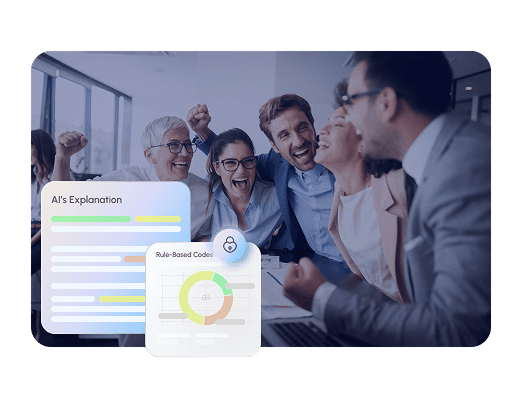
Transparent, Tailored, and Trusted AI Rationale
Our technology adapts to your organization's coding guidelines, evolving payer policies, and creates audit reports in real time
- Custom coding and denial rules per specialty or facility
- Clear and explainable AI decisions
- Adapt to new payer policies fast and with accuracy
Seamless Process Excellence
We architect integrated RCM solutions that ensure maximum revenue capture, continuous operational excellence and complete visibility
- Consistent and reliable outcomes across revenue cycle
- Proactive denial analytics
- Continuous learning from real-world feedback

Your Success Is Our Reputation
CombineHealth is a partner with proven revenue cycle expertise you can count on. With 40+ years of combined experience in healthcare revenue cycle and AI, we're a trusted platform for revenue cycle leaders.
Results we’re proud of


Internal Medicine

Critical Care

Pediatrics

Emergency Medicine

Anesthesiology

Dermatology

Neurology

Radiology

Psychiatry

Pathology

Family Medicine

Orthopedics

Gastroenterology

Ophthalmology

General Surgery

Obstetrics and Gynecology
Hematology and Oncology
Let’s work together and help you get paid
Book a call with our experts and we'll show you exactly how our AI works and what ROI you can expect in your revenue cycle.
Email: info@combinehealth.ai




















